Unveiling the mysteries of science can sometimes be as thrilling as a blockbuster movie. Our feature today delves into one such captivating topic: how vaccines work in strengthening our health and immunity. This comprehensive guide will walk you through the intricate details of the science behind vaccines, making it an essential read for anyone interested in understanding more about this life-saving technology. 🧪💉
In the wake of a global pandemic, there has never been a more critical time to understand the workings of vaccines. These microscopic warriors, working silently within our bodies, are often the unsung heroes in our fight against deadly diseases. This post aims to shed light on their mechanism of action, and how they help fortify our immune systems against a myriad of health threats.🦠🔬
Yet, vaccines are not just about combating viruses. They are also a testament to human ingenuity and the power of science. In this post, we will delve into the history of vaccines, their development, and how they have shaped our society’s health landscape. From the eradication of smallpox to the recent breakthroughs in mRNA technology, this post is a fascinating journey into the world of immunology.🧬🌐
Lastly, to truly appreciate the value of vaccines, we will be exploring the societal impact of vaccinations. Their role in promoting public health, increasing life expectancy, and fostering global development cannot be overstated. So, prepare to dive deep into the realm of vaccines – the tiny tools with massive impact on our health and immunity. Stay tuned!🌍🏥
Understanding the Core Principles of Vaccines
Vaccination is one of the most powerful tools in modern medicine. It has helped eradicate, control, and prevent the spread of numerous infectious diseases that once claimed millions of lives. But what actually happens when a vaccine is administered? To appreciate the science behind vaccines, it’s essential to understand how they interact with our immune system and how different types of vaccines function.
At its core, a vaccine trains the immune system to recognize and combat pathogens—like viruses or bacteria—without actually causing the disease. This is achieved by introducing a harmless component of the pathogen into the body, such as a protein, an inactivated version of the organism, or a piece of its genetic material. Once inside the body, the immune system treats this component as a threat and mounts a defense against it. This includes the production of specialized proteins known as antibodies.
Antibodies are part of the adaptive immune response. They are designed to recognize and bind to specific antigens—molecules on the surface of pathogens. When a person receives a vaccine, their immune system creates antibodies tailored to the particular disease-causing agent. If the vaccinated individual is later exposed to the real pathogen, their immune system can quickly recognize it and deploy these antibodies to neutralize the threat before it can cause illness.
But antibodies are only one part of the story. Equally important are memory cells—specialized white blood cells that remain in the body long after the initial exposure. These cells “remember” the specific pathogen, allowing the immune system to respond more swiftly and effectively if the body encounters it again. This memory-based response is what provides long-term immunity and is the cornerstone of how vaccines work.
There are several different types of vaccines, each utilizing a unique method to introduce antigens into the body:
-
Live attenuated vaccines contain a weakened version of the living pathogen. These vaccines are highly effective because they closely mimic a natural infection. Examples include the measles, mumps, and rubella (MMR) vaccine and the oral polio vaccine.
-
Inactivated vaccines use pathogens that have been killed or inactivated so they can no longer cause disease. These vaccines are stable and safe, especially for people with weakened immune systems. The inactivated polio vaccine and hepatitis A vaccine fall into this category.
-
Subunit, recombinant, and conjugate vaccines include only specific parts of the pathogen—often proteins or sugars—rather than the whole organism. These vaccines trigger a strong immune response with minimal risk of side effects. Examples include the HPV vaccine and the Haemophilus influenzae type b (Hib) vaccine.
-
Messenger RNA (mRNA) vaccines, a more recent innovation, work by providing genetic instructions for our cells to produce a harmless piece of the pathogen, such as the spike protein found in the coronavirus. Once produced, this protein triggers an immune response. The COVID-19 vaccines by Pfizer-BioNTech and Moderna are examples of mRNA vaccines.
-
Viral vector vaccines use a different virus (not the target pathogen) as a delivery system to introduce genetic material into cells. This instructs cells to produce antigens that stimulate an immune response. The Johnson & Johnson COVID-19 vaccine is one such example.
Ultimately, the goal of all vaccines is the same: to prepare the body’s immune system to recognize and combat disease-causing organisms before they can do serious harm. Through the creation of antibodies and memory cells, vaccines provide a safe and controlled way to build immunity, protecting individuals and, when widely used, entire communities from dangerous infections.
By understanding how vaccines work, we can better appreciate the science that protects us and contributes to healthier, longer lives for people around the world.
The Role of Memory Cells
Memory cells play a vital role in how vaccines protect the body from disease. These specialized immune cells are created after the body is exposed to a harmless form of a virus or bacteria through vaccination. Unlike the initial immune response, which takes time to build, memory cells remain in the body long after the vaccine is given.
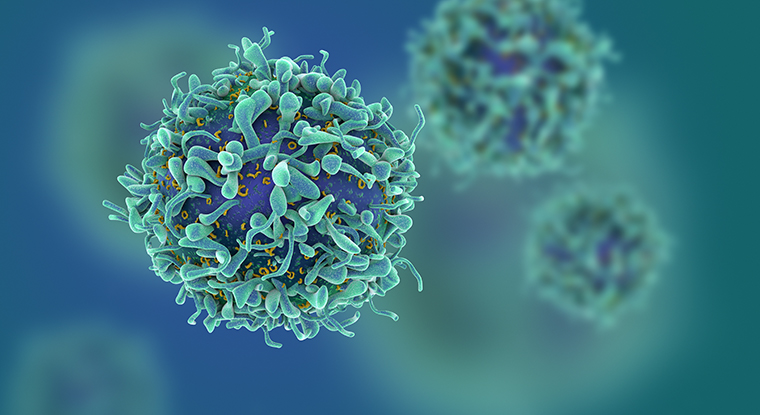
Their main job is to “remember” the specific pathogen. If the vaccinated person later encounters the real virus or bacteria, the memory cells recognize it instantly and trigger a rapid immune response. This quick action helps neutralize the threat before it can cause serious illness.
These cells can remain in the body for many years, sometimes even for life, depending on the vaccine. They are responsible for the long-term immunity that vaccines provide. In some cases, booster shots are used to remind the immune system and strengthen these memory responses. Thanks to memory cells, the body is not caught off guard when facing future infections—it’s already prepared to defend itself quickly and effectively.
Different Types of Vaccines
There are several types of vaccines, each designed to trigger an immune response in a different way. They include:
- Live attenuated vaccines: These vaccines use a weakened form of the germ that causes a disease. Examples include the measles, mumps, and rubella (MMR) vaccine and the chickenpox vaccine.
- Inactivated vaccines: These use a killed version of the germ. The flu shot is an example of this type of vaccine.
- Subunit, recombinant, and conjugate vaccines: These use specific pieces of the germ, such as its protein, sugar, or casing. This includes the HPV and Hepatitis B vaccines.
- Messenger RNA (mRNA) vaccines: A relatively new type of vaccine, mRNA vaccines teach cells how to make a protein that triggers an immune response. The COVID-19 vaccines from Pfizer-BioNTech and Moderna are examples of mRNA vaccines.
Immunity: Natural vs Vaccine-Induced
The primary goal of vaccination is to induce immunity without causing the disease itself. This is different from natural immunity, which is gained from actually getting the disease. Natural immunity can come with a heavy price – the disease may cause severe complications or even death.

On the other hand, vaccines use carefully selected antigens (substances that induce an immune response) from the disease-causing organism to stimulate the immune system. This means that vaccines provide the benefits of immunity without the risks associated with natural infection.
Hereditary Immunity: A Common Misconception
One of the most widespread misunderstandings in immunology is the belief that immunity can be inherited and passed down genetically through generations. While this idea seems logical at first glance—after all, many traits such as eye color or height are inherited—it doesn’t hold true when it comes to immunity in the way vaccines or infections confer protection.
The immune system does not transmit specific immunity to diseases from parent to child through DNA. Instead, what can be passed on genetically is the overall strength or responsiveness of the immune system, including certain predispositions to immune-related conditions. However, actual immunity to a disease—such as immunity to measles or the flu—must be acquired either through natural infection or vaccination during a person’s lifetime.
That said, there is a temporary and partial form of protection that newborns do receive, which likely contributes to this misconception. During pregnancy, mothers pass antibodies to their babies through the placenta. This is known as passive immunity, and it provides short-term protection during the first few months of life. Breastfeeding continues this process, as breast milk contains antibodies—especially Immunoglobulin A (IgA)—that help protect the infant from common infections.
However, passive immunity is not long-lasting. These maternal antibodies gradually decrease over time, usually disappearing by six to twelve months after birth. They do not result in the baby’s immune system “remembering” the pathogen or building its own defense, as happens with vaccine-induced or natural immunity.
In contrast, active immunity—the kind developed after vaccination or infection—involves the creation of memory cells that stay in the body for years, ready to respond to future encounters with the same pathogen. This type of immunity is personalized and cannot be transferred from one generation to the next.
In conclusion, while newborns benefit from a mother’s antibodies during early life, true immunity must be built individually. Understanding the difference between passive maternal protection and active long-term immunity helps clarify why vaccines are essential for every generation, even if their parents were immune.
Vaccines and Community Health
Vaccines not only protect the individuals who receive them but also contribute to community health. This concept, known as herd immunity or community immunity, occurs when a large percentage of a population becomes immune to a disease, making its spread unlikely. As a result, even people who can’t be vaccinated (such as those with certain health conditions) benefit from the protection provided by vaccines.
Vaccines have played a significant role in controlling, and in some cases, eradicating serious diseases. Smallpox, a deadly disease that once caused widespread devastation, has been eradicated globally thanks to vaccination. Other diseases, like polio and measles, have also been dramatically reduced or eliminated in many parts of the world.
Moreover, vaccines help reduce the burden on healthcare systems by preventing outbreaks and minimizing the need for hospitalizations and treatments. This not only saves lives but also conserves medical resources for other urgent conditions. In the face of pandemics, widespread vaccination is essential to restoring social and economic normalcy. Promoting vaccine equity across populations and countries is a crucial step toward achieving lasting global health security. By ensuring fair access to immunization, we build more resilient societies and protect the most vulnerable among us. Public trust, transparent communication, and strong healthcare infrastructure are also vital to sustaining long-term immunization efforts.
Conclusão
In conclusion, the science behind vaccines is both complex and fascinating. Vaccines are instrumental in bolstering our health and immunity, serving as a potent shield against infectious diseases. They work by stimulating our immune system to produce an immune response, essentially preparing our body for potential encounters with harmful pathogens. This immunological memory is a key component of how vaccines safeguard our health.
Moreover, vaccines not only protect individuals but also the community at large through herd immunity. This concept involves a significant portion of the population being immunized, which reduces the overall spread of disease and protects those who cannot be vaccinated.
While the process of developing a vaccine involves rigorous testing and thorough evaluation, the benefits that vaccines bring are immense. They have led to the eradication of diseases such as smallpox and a significant reduction in the prevalence of diseases like measles and polio.
Despite the challenges and controversies surrounding vaccination, the science is clear. Vaccines are a critical tool in our fight against infectious diseases. They save lives, reduce suffering, and protect our health and immunity. Therefore, embracing vaccines and understanding the science behind them is of paramount importance.